Concept Map Diabetes Mellitus Type 1: An in-depth examination of the pathophysiology, clinical manifestations, diagnosis, management, complications, and research advancements of Diabetes Mellitus Type 1, providing a comprehensive understanding of this prevalent condition.
Diabetes Mellitus Type 1, an autoimmune disorder characterized by the destruction of insulin-producing beta cells in the pancreas, leading to chronic hyperglycemia and a myriad of associated complications, demands a thorough understanding for effective management.
Definition of Diabetes Mellitus Type 1
Diabetes Mellitus Type 1 is a chronic autoimmune condition in which the body’s immune system mistakenly attacks and destroys the insulin-producing beta cells in the pancreas. Insulin is a hormone that helps glucose, or sugar, enter cells for energy production.
As a result of this destruction, people with Diabetes Mellitus Type 1 cannot produce insulin and must rely on insulin therapy to manage their blood glucose levels. Without insulin, glucose builds up in the blood, leading to a range of symptoms and potential complications.
Key Characteristics and Symptoms
The key characteristics and symptoms of Diabetes Mellitus Type 1 include:
- Frequent urination (polyuria)
- Excessive thirst (polydipsia)
- Increased hunger (polyphagia)
- Unexplained weight loss
- Fatigue
- Blurred vision
- Slow-healing sores
- Frequent infections
These symptoms typically develop over a short period of time, often within weeks or months. If you experience any of these symptoms, it is important to seek medical attention promptly for diagnosis and treatment.
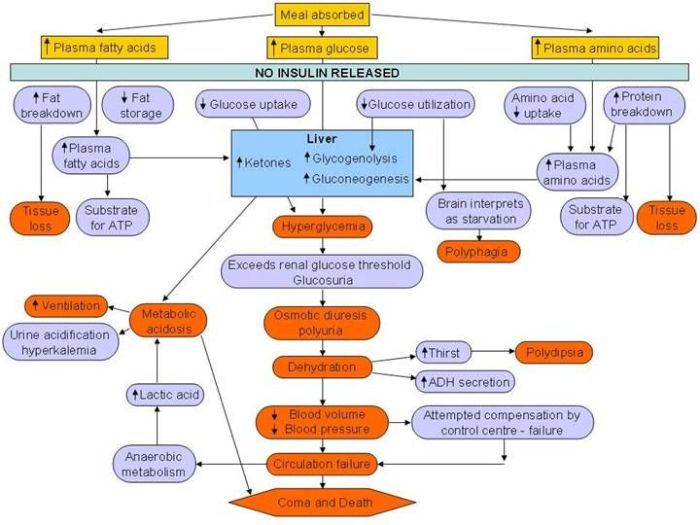
Pathophysiology of Diabetes Mellitus Type 1
Diabetes Mellitus Type 1 (T1DM) is an autoimmune disease characterized by the destruction of insulin-producing beta cells in the pancreas. This leads to an absolute deficiency of insulin, a hormone that is essential for glucose metabolism.
The exact cause of T1DM is unknown, but it is thought to involve a combination of genetic and environmental factors. In individuals with a genetic predisposition to T1DM, certain environmental triggers, such as viral infections or exposure to certain chemicals, may trigger the autoimmune response that leads to beta cell destruction.
Autoimmune Destruction of Beta Cells
The autoimmune response in T1DM is directed against the beta cells in the pancreas. These cells are responsible for producing insulin, a hormone that helps glucose enter cells for energy production.
In T1DM, the immune system mistakenly identifies the beta cells as foreign and attacks them. This attack leads to the destruction of beta cells and a decrease in insulin production.
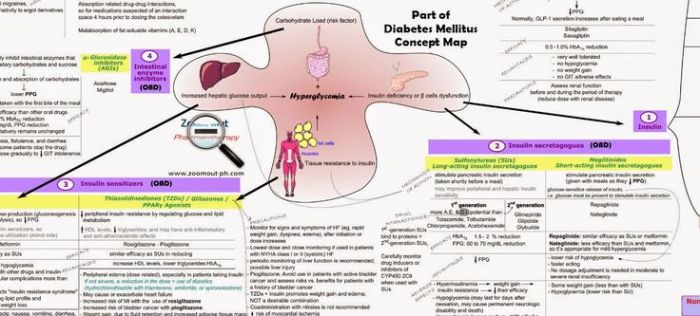
Hormonal Imbalances and Metabolic Disruptions, Concept map diabetes mellitus type 1
The absolute deficiency of insulin in T1DM leads to a number of hormonal imbalances and metabolic disruptions. These include:
- Hyperglycemia:The lack of insulin prevents glucose from entering cells, leading to high levels of glucose in the blood (hyperglycemia).
- Ketone production:In the absence of insulin, the body breaks down fat for energy, producing ketones. Ketones are acidic substances that can accumulate in the blood and cause ketoacidosis, a life-threatening condition.
- Weight loss:The body is unable to use glucose for energy, leading to weight loss.
- Polyuria:The high levels of glucose in the blood cause the kidneys to filter out more glucose, leading to increased urination (polyuria).
- Polydipsia:The increased urination leads to dehydration, which triggers thirst (polydipsia).
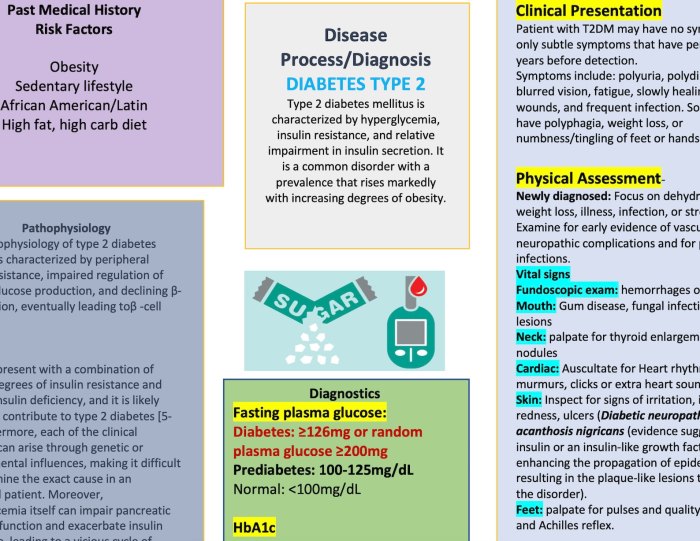
Clinical Manifestations of Diabetes Mellitus Type 1
Diabetes Mellitus Type 1, an autoimmune disease, presents with a distinct set of clinical manifestations. These symptoms arise due to the body’s inability to produce insulin, leading to elevated blood glucose levels (hyperglycemia) and a cascade of metabolic disturbances.
Hyperglycemia
- Elevated blood glucose levels are the hallmark of Diabetes Mellitus Type 1. Hyperglycemia occurs when the body cannot effectively utilize glucose for energy due to insulin deficiency.
- Chronic hyperglycemia can damage blood vessels and nerves, leading to long-term complications.
Polyuria
- Frequent urination is a common symptom of Diabetes Mellitus Type 1. The kidneys attempt to eliminate excess glucose from the blood by filtering it into the urine, resulting in increased urine volume.
- Polyuria can lead to dehydration and electrolyte imbalances if not managed properly.
Polydipsia
- Excessive thirst is another characteristic symptom of Diabetes Mellitus Type 1. The body attempts to compensate for fluid loss due to polyuria by increasing thirst.
- Unquenchable thirst can significantly impact daily life and well-being.
Polyphagia
- Increased hunger is a common manifestation of Diabetes Mellitus Type 1. Despite consuming adequate food, individuals with this condition may experience persistent hunger due to the body’s inability to utilize glucose for energy.
- Polyphagia can lead to weight loss and malnutrition if not addressed.
Potential Complications and Long-Term Effects
Untreated Diabetes Mellitus Type 1 can lead to a range of severe complications, including:
- Diabetic ketoacidosis (DKA): A life-threatening condition that occurs when the body breaks down fat for energy, producing ketones.
- Hypoglycemia: A condition characterized by dangerously low blood sugar levels.
- Retinopathy: Damage to the blood vessels in the retina, potentially leading to blindness.
- Nephropathy: Damage to the kidneys, potentially leading to kidney failure.
- Neuropathy: Damage to the nerves, causing numbness, tingling, and pain.
- Cardiovascular disease: Increased risk of heart attack and stroke.
Diagnosis of Diabetes Mellitus Type 1: Concept Map Diabetes Mellitus Type 1
The diagnosis of diabetes mellitus type 1 (T1DM) is established based on specific criteria and involves various tests to confirm the presence of the condition.
The diagnostic criteria for T1DM include:
- Classic symptoms of diabetes, such as polyuria (excessive urination), polydipsia (excessive thirst), and unexplained weight loss.
- Random blood glucose level of 200 mg/dL (11.1 mmol/L) or higher.
- Fasting blood glucose level of 126 mg/dL (7.0 mmol/L) or higher.
- Two-hour post-load blood glucose level of 200 mg/dL (11.1 mmol/L) or higher during an oral glucose tolerance test (OGTT).
- Glycated hemoglobin (HbA1c) level of 6.5% or higher.
In addition to these criteria, other tests may be performed to confirm the diagnosis of T1DM, such as:
- Autoantibody testing to detect the presence of antibodies against islet cells, which are the insulin-producing cells in the pancreas.
- C-peptide testing to measure the level of C-peptide, a byproduct of insulin production, which can help differentiate between T1DM and other types of diabetes.
Early diagnosis and timely intervention are crucial in managing T1DM effectively. Prompt diagnosis allows for the initiation of appropriate treatment, including insulin therapy, dietary modifications, and lifestyle changes, which can help prevent or delay the development of complications associated with the condition.
Management of Diabetes Mellitus Type 1
Management of diabetes mellitus type 1 involves a comprehensive approach that includes insulin therapy, blood glucose monitoring, lifestyle modifications, dietary management, and the utilization of technology. This multifaceted approach aims to maintain optimal blood glucose levels, prevent complications, and improve the overall well-being of individuals with diabetes.
Principles of Insulin Therapy
Insulin therapy is the cornerstone of diabetes management. It involves administering insulin, a hormone that facilitates glucose uptake into cells, to compensate for the body’s inability to produce sufficient insulin. There are various types of insulin available, each with its unique onset, peak, and duration of action.
Insulin dosing is individualized based on factors such as blood glucose levels, body weight, and activity level.
Blood Glucose Monitoring
Regular blood glucose monitoring is essential for effective diabetes management. It provides real-time information about blood glucose levels, allowing individuals to make informed decisions regarding insulin dosage, dietary intake, and physical activity. Various blood glucose monitoring devices are available, including glucometers and continuous glucose monitors.
Lifestyle Modifications
Lifestyle modifications play a significant role in diabetes management. Regular physical activity improves insulin sensitivity and helps control blood glucose levels. A balanced diet, low in refined carbohydrates and high in fiber, supports optimal blood glucose regulation. Adequate sleep, stress management, and smoking cessation are also important aspects of lifestyle management.
Role of Technology
Technological advancements have revolutionized diabetes management. Continuous glucose monitors (CGMs) provide continuous readings of blood glucose levels, allowing for real-time monitoring and early detection of glucose fluctuations. Insulin pumps deliver insulin in a more physiological manner, mimicking the body’s natural insulin secretion pattern.
These technological tools empower individuals with diabetes to manage their condition more effectively and improve their quality of life.
Complications of Diabetes Mellitus Type 1
Diabetes mellitus type 1 is associated with a range of acute and chronic complications that can significantly impact the health and well-being of individuals. Understanding the mechanisms and risk factors associated with these complications is crucial for effective prevention and management.
The complications of diabetes mellitus type 1 can be classified into two main categories: acute and chronic. Acute complications develop rapidly and require immediate medical attention, while chronic complications develop gradually over time and can lead to severe health problems if not properly managed.
Acute Complications
Acute complications of diabetes mellitus type 1 include hypoglycemia and diabetic ketoacidosis (DKA).
- Hypoglycemiaoccurs when blood glucose levels drop too low, typically below 70 mg/dL. Symptoms of hypoglycemia include shakiness, sweating, hunger, irritability, confusion, and seizures. Severe hypoglycemia can be life-threatening if not treated promptly.
- Diabetic ketoacidosis (DKA)is a serious complication that occurs when the body produces high levels of ketones in response to low insulin levels. Ketones are acidic substances that can build up in the blood and cause dehydration, electrolyte imbalances, and coma. DKA is a medical emergency and requires immediate treatment.
Chronic Complications
Chronic complications of diabetes mellitus type 1 include retinopathy, nephropathy, and neuropathy.
- Retinopathyis damage to the blood vessels in the retina, the light-sensitive tissue at the back of the eye. Retinopathy can lead to vision loss and blindness if not treated.
- Nephropathyis damage to the kidneys. Nephropathy can lead to kidney failure and the need for dialysis or a kidney transplant.
- Neuropathyis damage to the nerves. Neuropathy can cause numbness, tingling, pain, and weakness in the hands, feet, and other parts of the body.
The risk of developing complications from diabetes mellitus type 1 is influenced by several factors, including the duration of the disease, blood glucose control, blood pressure control, and lifestyle factors such as smoking and obesity. Regular monitoring of blood glucose levels, adherence to medication regimens, and lifestyle modifications are essential for preventing and managing complications.
Research and Advancements in Diabetes Mellitus Type 1
Ongoing research and advancements in Diabetes Mellitus Type 1 hold immense promise for improving the lives of individuals living with this condition. Scientists and researchers are actively exploring various approaches to enhance disease management, prevent complications, and ultimately find a cure.
Emerging Therapies
Several emerging therapies are gaining attention in the field of Diabetes Mellitus Type 1. These include:
- Islet Cell Transplantation:Involves transplanting healthy islet cells from a donor pancreas into the patient’s body. These cells can produce and release insulin, potentially restoring normal blood glucose levels.
- Stem Cell Therapy:Utilizes stem cells to generate insulin-producing cells. This approach aims to create a renewable source of insulin-producing cells, eliminating the need for external insulin administration.
- Gene Therapy:Seeks to modify the patient’s genes to enable their own cells to produce insulin. This approach has the potential to provide a long-term solution by correcting the underlying genetic defect.
Potential Impact
These emerging therapies have the potential to revolutionize the management and treatment of Diabetes Mellitus Type 1. Islet cell transplantation, if successful, could eliminate the need for insulin injections and significantly improve patients’ quality of life. Stem cell therapy and gene therapy, if proven effective, could potentially cure Diabetes Mellitus Type 1 by restoring the body’s ability to produce insulin naturally.
FAQ Summary
What is the primary cause of Diabetes Mellitus Type 1?
Diabetes Mellitus Type 1 is primarily caused by the autoimmune destruction of beta cells in the pancreas, leading to an absolute deficiency of insulin.
What are the characteristic symptoms of Diabetes Mellitus Type 1?
Classic symptoms include polyuria (excessive urination), polydipsia (excessive thirst), polyphagia (increased hunger), unexplained weight loss, and fatigue.
How is Diabetes Mellitus Type 1 diagnosed?
Diagnosis is established through blood tests, including fasting plasma glucose, random plasma glucose, or an oral glucose tolerance test, which measure blood sugar levels.
What are the potential long-term complications of Diabetes Mellitus Type 1?
Uncontrolled Diabetes Mellitus Type 1 can lead to severe complications, including retinopathy (eye damage), nephropathy (kidney damage), neuropathy (nerve damage), and cardiovascular disease.
What are the current research advancements in Diabetes Mellitus Type 1?
Ongoing research focuses on islet cell transplantation, stem cell therapy, gene therapy, and the development of artificial pancreas systems to improve insulin delivery and glycemic control.